California Governor Gavin Newsom has declared a state of emergency over the spread of avian influenza among dairy cows.
The statement signals growing concern about the situation in California, which has become the epicenter of the national outbreak of cattle.
In the past 30 days alone, more than 300 dairy herds in California have tested positive for the virus.
The governor said the confirmed infections in dairy cows on Southern California farms indicate the need for increased surveillance of the spread and a more coordinated response across the state.
“This declaration is focused on measures that will guarantee government agencies have the resources and flexibility they need,” Newsom said in a press release. “While the risk to the visible remains low, we will continue to take every measure possible to prevent the propagation of this virus.”
California currently accounts for about half of the known human infections in the United States.
There is no evidence of sustained human-to-human transmission in California or elsewhere. But scientists warn that uncontrolled spread in dairy cows could increase the risk of infection in humans and give the virus an opportunity to acquire dangerous mutations.
The measure also comes on the heels of another worrying development: the first case of severe symptoms in humans in this country.
On Wednesday, representatives of the Centers for Disease Control and Prevention announced further findings of the infection in a Louisiana resident who was hospitalized after coming into contact with sick and dead birds in his backyard flock.
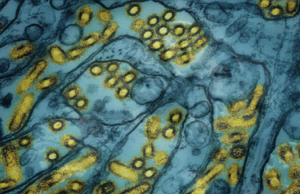
Genetic sequencing has shown that the H5N1 virus causing the disease belongs to a genetic lineage circulating among wild birds and poultry and is different from the virus that spreads to dairy cattle and causes the majority of infections in farm workers.
More than 60 people have been infected in the United States so far, but some studies suggest the official figures may be an underestimate.
The disease linked to dairy cattle mainly causes mild illness in humans.
The version of the virus in the Louisiana case is genotype D1.1. Infections previously surfaced among poultry workers in Washington State, who developed mild symptoms after testing positive in October. However, a teenager in British Columbia was recently hospitalized with the D1.1 strain of the virus.
Health Canada officials have not been able to determine how this person became infected.
The southwest Louisiana case was discovered during routine influenza surveillance and was eventually sent to the CDC for confirmation. The lawsuit does not change the CDC’s assessment that the risk to the public remains low.
But the hospitalization is a reminder that avian influenza has caused severe illness and death in other countries over the past 20 years, Dr. Demetre Daskalakis of the CDC told reporters at a news conference on Wednesday.
Daskalakis said his agency was conducting additional sequencing to look for worrying changes in the virus that could indicate it is evolving to become more transmissible or cause more severe illness.
Scientists were concerned that the British Columbia case had a specific mutation that could cause problems, but more research was needed to understand the exact impact.
Daskalakis referred reporters to Louisiana authorities, who are investigating the case, for more information on how the person may have contracted the virus and what symptoms he may have had.
As with the Louisiana infection, most cases have been traced to some kind of contact with sick animals. Milk from dairy cows contains large amounts of the virus, which is suspected to cause infection in farm workers. People who work with infected poultry can also become infected with the virus.
However, there have been several cases in the United States, including in California and Missouri, that have not been traced back to infected livestock. “In some cases, the source of infection is unclear, but in these cases, even in cases where contact with animals has been identified, human-to-human transmission has not been confirmed.” Daskalakis said.